Dental Crowns in Laguna Niguel
Effect of venting and seating techniques on the cementation of complete coverage restorations
(Originally was published in 1992)
M. A. Cruz, J. A. Sorenson, and W. K. Johnson
Clinical Relevance
The best seating of complete crowns during cementation can be
achieved by venting the crown and using a tapping cementation technique.
When the crown is not vented, a dynamic seating method provides the
best seating.
SUMMARY
Statement of Problem: The incomplete seating of crowns resulting from cementation phenomena is a universal problem for clinicians. This seating error may lead to disturbances in the occlusion, proximal contacts, reduced retention, and open margins. Various cementation protocols are practiced, with no established standard that maximizes crown seating and marginal fit.
Purpose: This study investigated the effect of various combinations of venting and cementation seating techniques with the routine use of die relief on the seating of complete gold crowns.
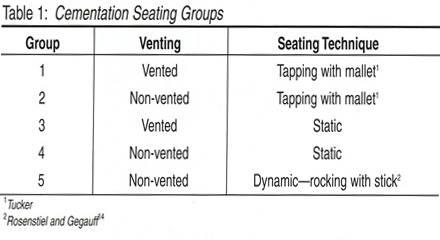
Material and Methods: Fifty human molars were prepared with a mounted handpiece for complete coverage crowns with a featheredge finish line and six degrees of taper, according to Tylman.39 Impressions were made, stone dies fabricated, die spacer was applied and the crowns were waxed and cast in type III gold. The respective crowns were placed on the teeth and preloaded. The distance between reference marks on the tooth and crown was measured at four points around each tooth. Zinc phosphate cement was mixed and the crowns were cemented in the following groups: 1) vented, tapping the crown into place with a mallet, 2) non-vented, tapping the crown into place, 3) vented static seating with a 25 kg load, 4) non-vented dynamic seating, 5) non-vented static loading with a 25 kg load. A25 kg load was then maintained on the crowns during the cement setting time. Distances between reference marks were then measured and the change in post-cementation distances calculated.
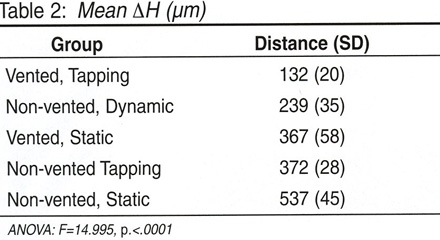
Results: ANOVA (F=14.995, p <.0001) and multiple range tests revealed significant differences between the groups. The mean increased post cementation distances for the seating groups were (µm): 1) 132 ± 20, 2) 372 ± 26, 3) 367 ± 59, 4)239 ± 35, 5) 537 ± 45.
Conclusions: The vented tapping technique produced the best seating. The non-vented tapping seating group produced seating not significantly different from the vented static method. The non-vented static group had the worst seating, with a gap four times greater than the vented tapping group.
INTRODUCTION
Failure to attain a completely seated crown during cementation may lead to disturbances in the occlusion interproximal contacts, decreased retention, open margins and, consequently, cement wash-out possibly leading to recurrent caries.1-2 There is general agreement in the literature regarding the virtues of venting, die spacing and dynamic seating as it relates to improved crown seating, but virtually no consensus on the optimal combination to use.3-9 This study investigated the effect of the routine use of die spacing with various combinations of non-static seating (tapping), static seating and dynamic seating techniques with vented and non-vented complete coverage restorations.
METHODS AND MATERIALS
Fifty molars were prepared with a high-speed handpiece and water spray mounted on a milling machine for complete gold crowns. An 860-014 bur (Brasseler USA, Savannah, GA, USA) was used to prepare a featheredge finish line and 6 degrees of taper according to Tylman and Malone.10 Impressions of the tooth preparations were immediately poured with 25 grams of Index Stone (Modern Materials, South Bend, IN, USA), which was pre-measured and mixed with 5.5cc of distilled water and mixed under vacuum. All stonecasts were placed in a chamber with 100% relative humidity to maximize the physical properties of the stone during setting. The dies were prepared with two coats of die spacer (Belle de St Claire, Encino, CA, USA), measuring ~22-26 µm on the axial walls to within1 mm of the margin and three coats on the occlusal surface, measuring ~33-39 µm.11 Waxing and casting procedures were followed according to Tucker12 to compensate for inherent expansion and shrinkage properties of the materials used in attaining precision castings, as described by Asgar and Clark.13 The 50 teeth with their respective crowns were randomly divided into five cementation seating groups of 10
Reference markings were made at the buccal, lingual, mesial and distal aspects approximately 1 mm from the margins on both the tooth and castings. Each crown was placed under a static load of 11.3 kg (25 lbs.) for 15seconds prior to pre-cementation measurements

Figure 1. Pre-cementation loading. made with a measuring microscope (Nikon, Tokyo, Japan). Three measurements were made at each of four points around the crown. Zinc phosphate cement (Flecks, Keystone, Cherry Hill, NJ, USA) was mixed in a standardized manner on a glass slab and applied to the casting with a cement spatula by filling approximately halfway. The mallet and seater (Suter Dental, Chico, CA, USA)
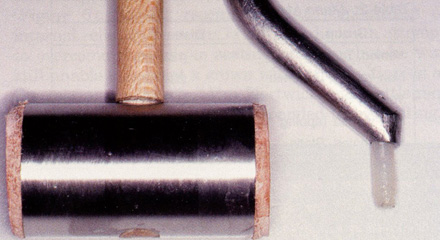
Figure 2. Mallet and Suter Seating instrument (contra-angle). were used to tap the crowns into place in the first two groups by applying the mallet force in various directions to assure full seating of the casting. This was continued with a moderate and clinically relevant force until no more cement extruded through the vent hole

Figure 3. Extrusion of cement through vent hole (tapping). and the crown was held with 11.3 kg of static pressure until complete cement cure. No vent pin was applied to the casting, as is customary in the clinical setting,7 due to the in vitro nature of the study. Groups 3 and 4 were seated with a static load of 11.3 kg after cement application as previously described, while Group 5 was dynamically seated as described by Rosensteil and Gegauff.14
All crowns were placed under a static load of 11.3 kg until completion of the cement cure

Figure 4. Extrusion of cement via dynamic seating. then placed in 100% humidity at 37C° for 10 minutes prior to placement in a water bath. Post-cementation measurements were again made three times at each of four points on each crown with a measuring microscope at100x magnification.
The mean pre- and post-cementation distances between the four reference marks were calculated for each crown. The mean change in height post-cementation was then calculated for each crown and the mean change in height was calculated for the five-cementation seating groups.
RESULTS:
ANOVA (F=14.995, p<.0001) and multiple range tests revealed significant differences between the groups
DISCUSSION: Often, the clinician works with focused diligence to prepare the tooth without causing pain to the patient, takes an accurate impression and finally fabricates the casting with precision only to give minimal consideration to the cementation procedure. Typically, the patient bites on a cotton roll or an orangewood stick while the cement cures, then the excess cement is removed. The literature suggests that this is the least desirable protocol to use when optimizing the seating of complete-coverage crowns. 14-15 The consequences have been previously mentioned. There is general agreement that open margins pose a risk factor for secondary decay; however, the occlusal considerations are often accepted as a clinical reality or overlooked altogether. It appears that gnathologic adjustment of extensive cases in fine-tuning the occlusion after remount procedures may be moot if there is a cementation error of higher magnitude.
In appreciating the significance of the cementation error, if one bites on a piece of articulating paper or a human hair (40-70 microns), its presence is perceived
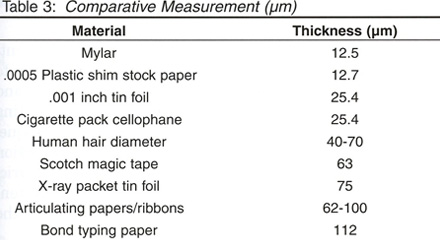
Therefore, it could be said that 100 microns are of clinical significance. In fact, there is a body of evidence to suggest that the human dentition is exquisitely sensitive to much finer tolerances and may accordingly alter gnathologic function.16-17
Although novel luting agents abound in the marketplace today and, as such, are more popular in use, zinc phosphate cement has been the standard in the profession and the only luting agent to receive a specification (No 8) from the National Bureau of Standards and the American Dental Association. It is specifically designed for the accurate seating of precision appliances.20 The ADA specification for the film thickness of type I zinc phosphate cement is 25 microns.20 As Pilo and others point out in their literature review on cementation, most investigations have found film thickness on cemented crowns to range from 60-435microns; the reason for such a wide range is manifold.21Eames states that we must face the fact that, under average conditions, our castings will be elevated 200microns on the prepared tooth.1 So, what is the correct cementation protocol to follow to predictably achieve an optimally seated full crown and mitigate the consequences? A systematic approach to reviewing the major considerations may prove useful.
Venting: The objection to venting techniques is unfortunately without basis. In fact, the importance of venting as described in the literature is significant. Cooper and others found that the venting of castings reduced the mean marginal opening by 45 microns,22 as did Van Nortwick and Gettleman, where the seating of crowns improved by 290 microns with venting.6 Kaufman and others showed a retention increase between 19% and 32% while improving seating by 175 microns.23 The use of venting and die spacing allows for optimal compensation of the hydrodynamic phenomena while assuring a uniform distribution of the luting agent. As Dimashkieh and others found, the time of final seating with venting was reduced from 60 seconds to 15 seconds, thus preventing the restriction of cement flow due to curing viscosity.24 Van Nortwick and Gettleman found that the combination of venting and internal relief seated full crowns more accurately than with either alone.6 Jorgensen considered the hydrodynamic condition created during cementation as the primary consideration to overcome in obtaining the thinnest cement film thickness.25 Hoard and others describe venting as working because it affects the flow, limits the stacking of the particles and relieves residual intracoronary pressure. 3 Therefore, with these findings, why is venting not routinely used? Some possible explanations include the notion that venting requires an extra visit to fill the vent hole or that the vent hole may display marginal micro-leakage resulting from the vent opening.11 Bassett previously described a technique that requires a little more than 90 seconds of additional labor.7 The amount of time required to adjust the occlusion properly due to seating errors may run an order of magnitude greater if venting is not used, while still having a compromised margin seal. Plastic analog pins are sprued and cast out of a type 4 gold. After the cement has been vented, the pin is placed in the vent hole, malleted into place, then cut with a diamond disc or round bur. The remaining pin tag is removed and polished with traditional finishing discs. The vent hole is sealed and is not evident to the naked eye. One last compelling reason to routinely use venting was theorized by Bergenholtz and Nyman.26 The hydrodynamic pressure that deforms the crown may also act on the pulp through the porous dentin, which, in turn, may transport some cement constituents into contact with vital tissue. This effect may have adverse consequences on the pulp, ranging from transient pulpal inflammation to pulpal necrosis. In the aforementioned study, it was found that, over a mean observation period of eight years, 9% of teeth receiving crown restorations required root canal therapy with no obvious cause. This incidence of approximately 1% of crowned teeth requiring root canal therapy per year has been confirmed in other studies and maybe a delayed consequence of pulp damage from intra-cementation pressure generation.26-28
Seating Techniques: Jorgenson discussed the phenomena of obliquity, stating that it was impossible to seat a full casting without some degree of obliquity or tilt even when vented25
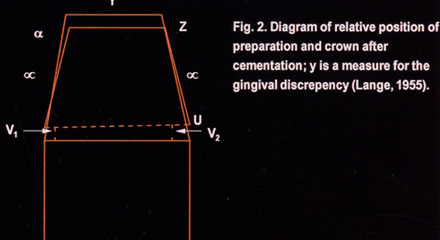
recommended a combination of internal relief and venting of the test die in an attempt to overcome the oblique seating problem, but he was still unable to cement a crown without some tipping of the casting on the die.7 Van Nortwick and Gettleman found that closer seating corresponded to less tilting.6 The current investigation suggests that an alternative seating technique, such as mallet tapping in combination with venting and die relief, will predictably overcome the obliquity phenomena. Mallet tapping allows for uniform seating by directing the seating force at various angles to the long axis of the tooth, thus overcoming the tendency of the crown to hang up on any particular preparation wall. Regarding the use of other non-static seating techniques, Koyano and others found that vibration during cementation produced a thinner cement film at the margins of the restorations than static pressure alone.5 Oliveira and others found that vibration improved the adaptation of MOD inlays.24 Ishikiriama and others found that the mechanical vibration of crowns at cementation promotes a better fit.4
Axial Fit
Since 1932, more than a dozen gold casting procedures and techniques have been introduced to the dental profession.3 The main motive for developing and introducing these techniques is to produce a metallic replacement for missing tooth structure as accurately and easily as possible. An exact tolerance for acceptance or rejection of any dental casting has not been determined.13 In fact, in the literature relating to dying relief, venting, cement, and cementation techniques, it is assumed that the castings fit the die and/or tooth accurately and, as such, are subjective.13,30-31 It is apparent that a wide spectrum exists as to the amount of compensation that is taken in making the castings fit on dies, which obviously should affect our comparisons from one study to the next. It seems that the lack of consistency in the literature in accounting for the inaccuracies inherent with the lost wax technique allows for a flawed comparison from one study to the next when evaluating film thickness/margin closure. In his study, Byrne discussed looking at the influence of finish-line form on crown cementation, the subject of internal or axial fit of castings as not having received much attention in the literature.9 He further mentions the difficulty in defining satisfactory casting adaptation for laboratory and clinical purposes. “In general, studies of cemented casting adaptation have only examined occlusal and marginal displacement, while ignoring axial wall adaptation.” Fusayama and others found that the thickness of zinc phosphate cement for optimum shear strength was 31-38 microns.32-33 Vermilyea and others found that the advantage of high shear strength provided by zinc phosphate cement is compromised by cementing oversized full coverage castings.14Thus, the use of zinc phosphate for “precision” castings, as indicated by ADA specification number 8,20 diminishes if the casting is not precise and perhaps would be better off with one of the newer cement whose micro-leakage and bonding properties are proven to be superior. In summary, the routine use of die spacing with venting and mallet tapping affords the best opportunity to attain optimal margin closure. By understanding and following a strict laboratory protocol in compensating for the inaccuracies of the lost wax casting technique, one is able to concurrently achieve maximal retention via 1) primary retention at the margin through frictional accuracy of the casting and 2) secondary retention via cohesive friction along the axial wall from the cement.
The proven long-term history and superior shear strength of zinc phosphate is optimized due to the accuracy of the axial fit, further enhancing retention. All of this combines for predictable longevity and occlusal harmony. Although the 3-degree taper per side used in this study was maximal, as described by Tylman,10 its clinical relevance is questionable. In fact, in the clinical situation where less taper is applied to the preparation technique, the cementation error is significantly minimized without compromising axial fit or retention, and one should expect significantly lower margin discrepancy numbers than was reported in the current study. When using the hygroscopic expansion casting technique, the decreased taper allows for a more favorable water/powder ratio in attaining accurate expansion of the wax pattern invested and, as such, fits the tooth more accurately.12 The cementation technique described must be used, however, to attain the most favorable result. Further investigation is necessary to determine the amount of achievable taper in a clinical setting without compromising the desired result.
CONCLUSIONS
- The use of venting and tapping resulted in the best marginal closure compared to the other groups.
- The non-vented static group resulted in the least desirable margin closure.
- There was no statistically significant difference between the non-vented tapping group and the static vented group.
References
- Eames WB (1981) The casting misfit: How to cope The Journal of Prosthetic Dentistry 45(3) 283-285.
- Assif D, Azoulay S & Gorfil C (1992) The degree of zinc phosphate cement coverage of complete crown preparations and its effect on crown retention The Journal of Prosthetic Dentistry 68(2) 275-278.695.
- Hoard RJ, Caputo AA, Contino RM & Koenig ME (1978) Intra-coronal pressure during crown cementation The Journal of Prosthetic Dentistry 40(5) 520-525.
- Ishikiriama A, Oliveira JF, Viera DF & Mondelli J (1981) Influence of some factors on the fit of cemented crowns The Journal of Prosthetic Dentistry 45(4) 400-404.
- Koyano E, Iwaku M & Fusayama T (1978) Pressuring techniques and cement thickness for cast restorations The Journal of Prosthetic Dentistry 40(5) 544-548.
- Van Nortwick WT & Gettleman L (198l) Effects of internal relief, vibration, and venting on the vertical seating of cemented crowns The Journal of Prosthetic Dentistry 45(4) 395-399.
- Bassett RW (1966) Solving the problems of cementing the full veneer cast gold crowns The Journal of Prosthetic Dentistry 16(4) 740-747.
- Wang CJ, Millstein PL & Nathanson D (1992) Effects of cement, cement space, marginal design, seating aid materials, and seating force on crown cementation The Journal of Prosthetic Dentistry 67(6) 786-790.
- Byrne G (1992) Influence of finish-line form on crown cementation The International Journal of Prosthodontics 5(2) 137-144.
- Tylman SD & Malone WFP (1978) Tylman’s Theory and Practice of Fixed Prosthodontics 7th ed The CV Mosby Company St Louis 105-108.
- Campagni WV, Preston JD & Reisbick MH (1982) Measurement of paint-on die spacers used for casting relief The Journal of Prosthetic Dentistry 47(6) 606-611.
- www.rvtucker.org.
- Asgar K & Clark S (1976) Clinical Dentistry Harper & Row Publishers Hagerstown 1-20.
- Rosenstiel SF & Gegauff AG (1988) Improving the cementation of complete cast crowns: A comparison of static and dynamic seating methods Journal of the American Dental Association 117(7) 845-848.
- Gegauff, AG & Rosenstiel, SF (1989) Reassessment of die spacer with dynamic loading during cementation The Journal of Prosthetic Dentistry 61(6) 655-658.
- Levy JH, Robertson LT, Dong WK & Petrisor D (2001) Tactile thresholds of human incisors at two frequencies Journal of Dental Research 80 174.
- Petrisor D, Levy JH & Robertson LT (2002) Tactile thresholds of human maxillary and mandibular incisors Journal of Dental Research 81 397.
- Levy JH, Robertson LT, Lilly DJ, Petrisor D & Dong WK(2002) Possible role of interdental afferents in the mechanoreception of tooth contacts in humans Journal of Dental Research 81 396.
- Robertson LT, Levy JH, Petrisor D, Lilly DJ & Dong WK(2003) Vibration perception thresholds of human maxillary and mandibular central incisors Archives of Oral Biology48(4) 309-316.
- Council on Dental Materials and Devices: Specification No 8for zinc phosphate cement (1978) Journal of the American Dental Association 96 121.
- Pilo R, Cardash HS, Baharav H & Helft M (1988) Incomplete seating of cemented crowns: A literature review The Journal of Prosthetic Dentistry 59(4) 429-433.
- Cooper TM, Christensen GJ, Laswell HR & Baxter R (1971) Effect of venting on cast gold full crowns and inlays The Journal of Prosthetic Dentistry 26(6) 621-626.
- Kaufman EG, Coelho DH & Colin L (1961) Factors influencing the retention of cemented gold castings The Journal of Prosthetic Dentistry 11(3) 487-502.
- Dimashkieh MR, Davies EH & Von Fraunhofer JA (1974) Measurement of the cement film thickness beneath full-crown restorations British Dental Journal 137(7) 281-284.
- Jorgensen KD (1960) Factors affecting the film thickness of zinc phosphate cements Acta Odontologica Scandinavica18(4) 479-490.
- Bergenholtz G & Nyman S (1984) Endodontic complications following periodontal and prosthetic treatment of patients with advanced periodontal disease Journal of Periodontology55 (2) 63-68.
- Jackson CR, Skidmore AE & Rice RT (1992) Pulpal evaluation of teeth restored with fixed prostheses The Journal of Prosthetic Dentistry 67(3) 323-325.
- Cheung GS (1991) Preliminary investigation into the longevity and causes of failure of single unit extra coronal restorations Journal of Dentistry 19(3) 160-163.
- de Freitas Oliveira F, Ishikiriama A, Vieira DF & Mondelli J(1979) Influence of pressure and vibration during cementation The Journal of Prosthetic Dentistry 1979 41(2) 173-177.
- Kasloff Z (1961) Casting techniques and some variables The Journal of Prosthetic Dentistry 11(3) 533-536.
- Eames WB, O’Neal SJ, Monteiro J, Miller C, Roan JD Jr &Cohen KS (1978) Techniques to improve the seating of castings Journal of the American Dental Association 96(3) 432-437.
- Fusayama T & Iwamoto T (1961) Optimum cement film thickness for maximum shear resistance between teeth and restorations Bulletin of Tokyo Medicine and Dental University 8 147.
- Fusayama T, Ide K, Kurosu A & Hosoda H (1963) Cement thickness between cast restorations and preparation walls The Journal of Prosthetic Dentistry 13(2) 354-364.
- Vermilyea SG, Kuffler MJ & Huget EF (1983). The effect of die relief agent on the retention of full coverage castings The Journal of Prosthetic Dentistry 50(2) 207-210





